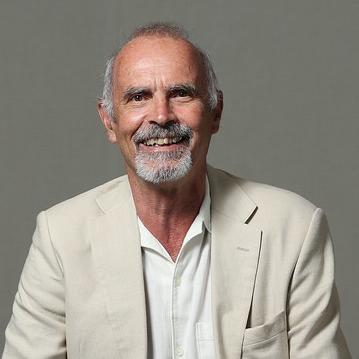
Ahead of National Diabetes Month in November, we sat down with Dr. Ian Scobie, assistant clinical dean, American University of the Caribbean School of Medicine (AUC), United Kingdom (AUC U.K. Track). Dr. Scobie is an expert on diabetes and a Fellow of the Royal College of Physicians (FRCP). He trained clinically in general medicine, endocrinology, and diabetes, and is now retired from the United Kingdom National Health Service. Dr. Scobie has written extensively on diabetes, including An Atlas of Diabetes Mellitus, which he is currently revising for its fourth edition.
Diabetes, a disease caused by abnormally high blood glucose (blood sugar), affects some 37 million people in the United States and hundreds of millions of people worldwide. Diabetes can damage the eyes, heart, kidneys, and nerves, and it is linked to various cancers.
Q: What are the types of diabetes?
A: Type 2 diabetes is the disease’s most common form. In Type 2 diabetes, cells don’t respond normally to insulin, which helps the body use or store blood glucose. This results in high blood sugar levels that can damage the body and cause serious health problems. In Type 1 diabetes, the pancreas makes insufficient insulin or none at all. Without insulin, blood sugar can’t get into cells and it builds up in the bloodstream. Type 1 diabetes was once called juvenile diabetes because it most often affects children. We must also mention prediabetes, a condition where blood sugar levels are higher than they should be, but not yet high enough to qualify as Type 2 diabetes.
Q: Are there effective ways to prevent and treat diabetes?
A: We cannot prevent Type 1 diabetes, which is naturally occurring, brought on mainly by genetics or certain viruses — but it can be treated successfully. Those affected by the disease must manage the amount of sugar in the blood through a healthy diet, insulin administration, and a healthy lifestyle to help prevent complications.
Type 2 diabetes risk factors include obesity and an unhealthy diet and lifestyle, so yes, it can be prevented. Eating and living well, getting enough exercise — these things can help prevent Type 2 diabetes. But other risk factors — such as age, ethnicity, family history, and race — are beyond our control. Treatments may deal with diet and exercise, therapies targeting insulin sensitivity or secretion, insulin or drug administration, and even surgery in some cases.
For people who are prediabetic, the key thing to do to reverse the condition or prevent progression to frank diabetes is to alter their lifestyle with particular emphasis on weight loss, a healthy diet, and physical exercise.
Q: When should people be screened for diabetes?
A: Screening for diabetes is important and simple. Screening for Type 2 diabetes, which involves blood sugar tests, often begins around age 35, but all overweight adults or those who experience diabetes symptoms should be screened. Blood tests for Type 1 diabetes are recommended for people who have family members with the disease, or for those with diabetic symptoms.
Q: Are there new developments in diabetes research?
A: There are too many developments to mention them all, but two areas have been monumental in their impact: new innovative drugs for the treatment of Type 2 diabetes, and systems to allow continuous noninvasive monitoring of blood glucose levels for patients with Type 1 diabetes and others treated with insulin.
Q: Is there a cure for diabetes?
A: There is no cure for diabetes. For now, Type 2 diabetes may be tempered through weight management, healthy lifestyle changes, and a range of drugs. These aren’t cures, but they can reduce the dangers of Type 2 diabetes or even put it into remission. Type 1 diabetes is trickier, and a cure would involve disrupting the immune system’s attack on beta cells — or replacing the beta cells altogether. [Beta cells make insulin, the hormone that controls glucose levels in the blood.] We can’t yet do that, but immunotherapies have shown the ability to briefly delay the onset of Type 1 diabetes, and beta cell transplants — which require donated pancreases — have proved briefly effective. Perhaps in the future, we could stop people from ever developing Type 1 diabetes, something we cannot do for Type 2 because it is so closely related to lifestyle factors.
Q: You are an endocrinologist. How does that figure into diabetes treatment?
A: Endocrinologists specialize in the diagnosis and treatment of hormone-related diseases and conditions, of which diabetes is one. The disease is essentially an imbalance of the hormone insulin, so endocrinologists are often experts in the different kinds of diabetes as well as obesity, thyroid dysfunction, and other metabolic conditions and disorders. As endocrinologists, we determine treatments for diabetes and help patients make healthy lifestyle changes.
Q: What drew you to endocrinology and diabetes?
A: At first, as with so many professional inspirations, a charismatic leader and a golden opportunity. But I like endocrinology, solving the enigmas of hormonal disorders, and putting together the pieces to arrive at a correct diagnosis. It is an intellectual challenge, putting all the jigsaw pieces in the right places to solve problems. It never fails to excite. As for specializing in diabetes, it’s a natural progression for an endocrinologist. I find it rewarding to help patients manage and cope with a long-term condition that can affect many aspects of their lives.
Q: What brought you to AUC?
A: I was initially approached — way back in 2003 — to become a site director at my hospital when AUC was looking for U.K. sites. Several years later, I was delighted to respond to the search for a U.K. assistant dean. I enjoy teaching and the educational environment. I’ve always identified with young people, and I find it rewarding to help and support them on their medical and life journey.
Visit the National Library of Medicine bookshelf to learn more about Type 1, Type 2, and other forms of diabetes. For more on National Diabetes Month, visit the National Institute of Diabetes and Digestive and Kidney Diseases, and check out their awareness toolkit.
At AUC School of Medicine, we’re training future endocrinologists and other specialist physicians. Our 2022–2023 MD graduates achieved a 97% first-time residency attainment rate and are now beginning their postgraduate training across 24 specialties.* Learn more about AUC and its MD program, as well as Dr. Scobie and the rest of our faculty and staff. Cheers, Dr. Scobie. We appreciate your time!
*Percentage of students attaining a 2023–2024 residency position out of all graduates or expected graduates in 2022–2023 who were active applicants in the 2023 NRMP match or who attained a residency position outside the NRMP match.