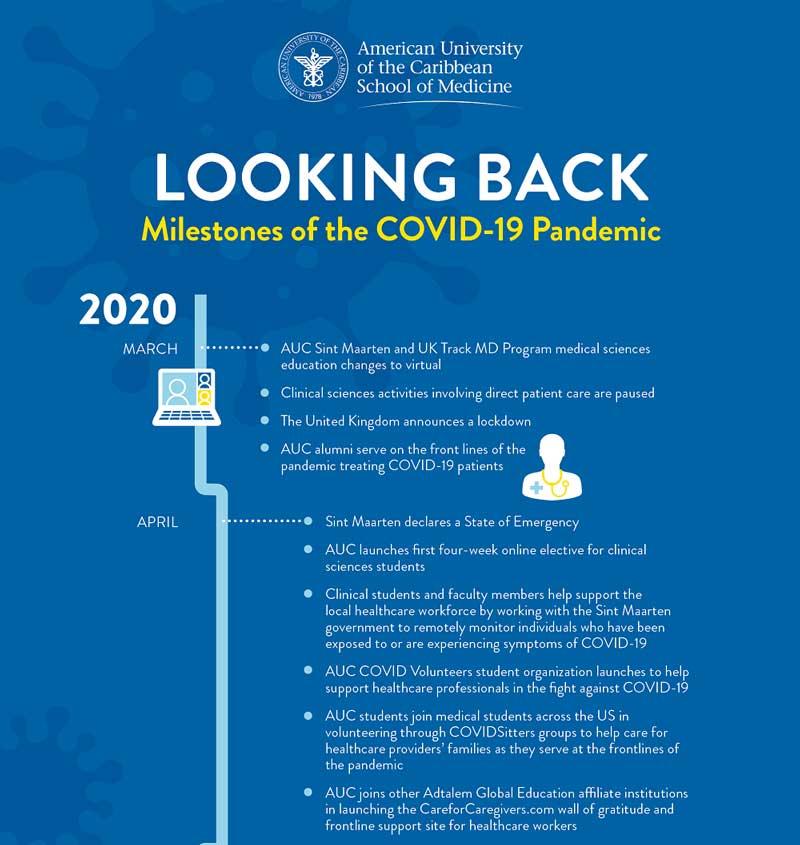
As I engage in discussions with our clinical partners and colleagues in various health care settings, I am learning the very different ways in which health care workers and health care systems responded to COVID-19. One element, however, is universal – no health care setting looks like it did before COVID-19. As we prepare to send our clinical students back into clinical rotations, I wanted to share some thoughts on those common differences.
Some of you, like myself, were once on the frontlines and many of you will soon be there—but we are experiencing this pandemic differently than our colleagues who have continued to treat patients over the past few months. Remember Hurricane Irma. When the category 5 hurricane hit Sint Maarten, we bonded over one of the most intense tropical cyclones in recorded history. But as an event, Irma was very different for the students, faculty and staff who weathered the storm on island compared to those of us who endured it from afar. As medical students and medical educators, we are experiencing the COVID-19 pandemic in a similar fashion.
I raise this for our clinical students who will soon resume hospital clerkships at sites that have been through an extremely traumatic time. What and who you return to will look and feel differently from the places you left in March. It’s going to be crucial for you to take the past months’ events into consideration as you arrive to the hospital, and be sensitive to the environment in which you are entering. Seek to understand the experiences of all members of the health care team.
What should you expect? You will encounter many people who are tired, overwhelmed, and who have been working continuously under a high-stress environment. People cope with stress in different ways, some may seek out opportunities to talk about the pandemic, others may avoid it altogether; and some may be moody or irritable. Just remember to approach your interactions with understanding and equanimity.
You will also see new processes and policies that have been put in place to prepare for a local outbreak and to protect patients and providers from the virus. Hospitals have changed the way their waiting rooms look and function, how elective procedures are being handled, how PPE is used, how and when patients’ symptoms are monitored, and visitor policies. Many health care systems are finding innovative ways to connect with the community, whether through outreach programs or mobile/telemedicine offerings. Take in these changes and pay attention to how your clinical site has adjusted to deal with a number of pandemic-related challenges. In one sense this pandemic is an excellent real-time example of Quality Improvement (QI) principles in action.
It’s also normal to feel anxious as you return. Some students have expressed concern about being rusty after not being physically present with patients and attendings. Don’t worry, you will quickly surpass where you were before. You may also be working with patients in ways that are new to you. You will adapt, and I have no doubt that you will pick up these new ways of providing care. And, you may even experience something unexpected – sadness, for instance, when working with patients who are dying without their loved ones physically present. Please reach out to your wellness counselors who are here to help you process these situations. Importantly, be open to the new experiences and opportunities that will emerge from this pandemic. It’s in times like these that we can learn the most.
Heidi Chumley, MD, MBA
Provost